High-speed motor vehicle accidents provide the sufficient force to cause fractures to the pelvis and considering that the forces are also delivered to other parts of the body other associated injuries are often present. Fifty percent of deaths with pelvis fractures are related to uncontrolled pelvic bleeding and the rest are related to the associated injuries that lead to sepsis, multi-organ failure, brain injuries, and pulmonary embolism.
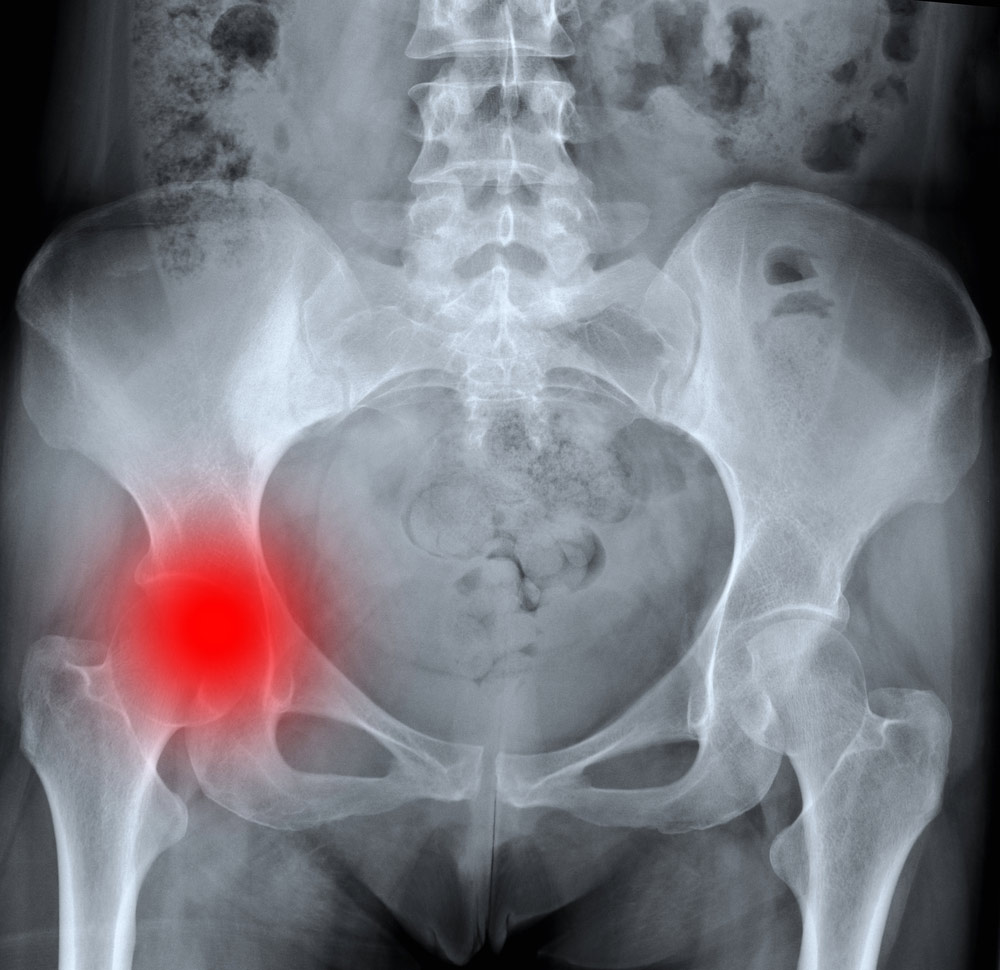
For patients who suffer a posterior hip dislocation with a displaced fracture of the acetabulum (hip socket), timing of repair is often determined by associated injuries A study from a major trauma center in Los Angeles involving over 100 patients with fractures of the acetabulum and a concomitant posterior dislocation of the hip indicate that the quality of the surgical ‘reduction’ or putting the fracture fragments together via plates and screws is the most important factor that determines future function and complications requiring other procedures such as total hip replacements. Therefore, once the patient is stable it is often prudent that the patient is transferred to a medical facility with experienced Orthopedic Trauma Surgeons who specialize in this technically challenging procedure.
Anatomic reduction of the fracture fragments with less than 2 millimeters deviation from anatomic alignment is considered excellent, but does not alone guarantee a good functional outcome. Other factors related to the original injury such as damage to the femoral head, impaction of the cartilage and bony cup of the acetabulum, and if the cup has multiple fragments of bone that needs to be reduced. Unlike an isolated posterior hip dislocation where early reduction within six hours is necessary to prevent decreased blood supply to the femoral head causing avascular necrosis (AVN), this is not nearly a problem in posterior dislocations with an acetabulum fracture since the blood supply isn’t compromised as much as it is with a pure dislocation.
Acetabulum fractures regardless of the severity have long lasting impacts on the patient’s function. Studies indicate that individuals with ‘simple’ fractures of the posterior wall have significant functional deficits compared to those without and those that involve the posterior ‘column’ have even worse a prognosis. Even with a ‘successful’ subsequent total hip replacement functionally these individuals remain impaired compared to similarly aged people. In the elderly with osteoporosis and those with advanced arthritis who suffer a posterior wall fracture may benefit from immediate total hip replacement since this procedure may provide a superior result than attempts at internal fixation.
Understanding the need for superior operative management to optimize outcomes the injured need early referrals to experienced Orthopedic Trauma Surgeon at a Level 1 or Level 2 Trauma Center where associated injuries can be managed and a well planned repair of the acetabulum be provided. Case Managers must refer these patients to acute rehabilitation for a minimum of three to four weeks where they receive the benefit of daily physician exams that will allow for timely identification and treatment of potential complications including the dreaded post-operative infection involving the acetabulum. This is a life-threatening problem that often requires complete removal of implanted hardware, prolonged wound care, nutritional support, surgical debridement, prolonged IV antibiotics, and plastic-reconstructive surgery.
Life Care Planners must use both treating physicians and experts in Orthopedic Trauma Surgery to understand prognosis and future care requirements as one ages with this disabling injury because even with excellent reduction of the fragments avascular necrosis, heterotopic ossification, and the need for early total joint replacement is not unusual.
Complications include avascular necrosis, heterotopic ossification, and the need for an early total joint replacement was not unusual.
http://emedicine.medscape.com/article/385838-overview
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1358569/
http://www.bjj.boneandjoint.org.uk/content/87-B/1/2.short
http://www.bjj.boneandjoint.org.uk/content/88-B/6/776.short
http://www.bjj.boneandjoint.org.uk/content/88-B/12/1618.short
Press Contact
Dr. Greg Vigna, MD, JD
T: 800-761-9206
https://www.lifecare123.com
Connect with Dr. Greg Vigna, MD, JD
on Facebook, Twitter, or Google+
#DrGregVigna

